The symposium of 2019, From Bench to Bedside, took place on the 21nd and 22th of November 2019.
This sympossium focussed on the different stages of scientific research and how research is used to develop new ways of tratment and can impact on public health, both in the infection and immunological fields.
Speakers:
Prof. Dr.  Liam O’Mahony
Liam O’Mahony
Principal Investigator Molecular Immunology at the Swiss Institute of Allergy and Asthma Research and Professor ofImmunology at APC Microbiome Ireland.
The Roles of Microbes and their Metabolites in Allergic Immune Responses
The influence of microbiome composition and metabolic activities on human health throughout life is, by now, a well-established research and clinical concept. Significant progress has been made on elucidating these interactions, but there are still many unresolved and challenging questions remaining. In this presentation, I will provide an overview of the fundamentals of mucosal immunological responses to microbes and how our understanding of this field has changed in recent years. In addition, I will review microbiome/host interactions and the mechanisms by which these interactions influence allergic responses. Finally, I will identify the areas where we need to focus our future basic research activities in order to progress the clinical understanding of the microbiome’s influence on health, especially in immune development and allergy prevention.
Prof. Dr. Jeffrey Beekman
Professor Cellular Disease Models and Principal Investigator of Cystic Fibrosis research lab of the Department of Pediatrics at University Medical Center Utrecht.
Intestinal organoids and the modelling of CF disease
Prof. Beekmans lab aims to develop cellular disease models that capture human disease and therapy thereof. Such models are used in a preclinical context to identify new biology, new treatment options or mode-of-actions of treatments for various genetic diseases. In the clinical domain, we explore how patient cells can be used as a living biomarker to support individual clinical decision making (e.g. personalized treatment) or to help stratify patients for clinical trials with new drug candidates. His research has focussed on cystic fibrosis, but is currently expanding to other genetic diseases. Cystic fibrosis is a genetic disease that affects epithelial defence mechanisms against pathogens, which lead to chronic infections of the lungs and strongly reduced quality of life and life expectancy. New treatments that target the root cause are being developed, but their exact mode of actions and individual efficacy remain unclear. His work on intestinal organoids and the modelling of CF disease showed for the first time that biobanks of patient-derived stem cell cultures could be used to identify patients with rare variants of CF that could benefit from these treatments, leading to individual access and reimbursement. This work has been awarded by multiple prestigious international awards, and the application of organoids for personalized medicine of CF is currently implemented worldwide.
Prof. Dr. Leo James
Principal Investigator MRC, Medical Research Council Laboratory of Molecular Biology at the University of Cambridge.
Trim-Away: Targeted degradation of pathogens and proteins by the cytosolic antibody receptor TRIM21
Viruses are masters of rapid change, adapting and evolving within days. In contrast, our immune system evolves slowly over decades. Antibodies are the exception to this rule and the only molecule we make that targets viruses and evolves on the same timescale. But viruses have a second trick; they replicate inside our cells and away from antibodies circulating in the blood. At least this was the view for over a century. In my talk, I will describe the recent discovery that there is a system of intracellular antibody immunity that protects us from infection. During infection, antibodies stick to circulating viruses and accompany them into cells. Once inside the cell, antibody-coated viruses are detected by an enzyme called TRIM21. TRIM21 tags each virus for destruction in the proteasome, the cell’s recycling machine. TRIM21 is found in every cell in the body, ready to destroy not only diverse viruses but also proteopathic neurodegenerative agents like tau. I will discuss how we are learning about this system in order to better understand infection and inspire new therapeutics and biotechnology. An example of this is ‘Trim-Away’, a technology in which TRIM21 is used to rapidly degrade specific cell proteins instead of viruses. This technology offers an alternative to siRNA or CRISPR but with the advantage that it removes existing proteins within hours. While Trim-Away is currently used as a research tool, it could be adapted in the future into a new type of therapeutic to treat a wide range of diseases.
Prof. Dr. Willem 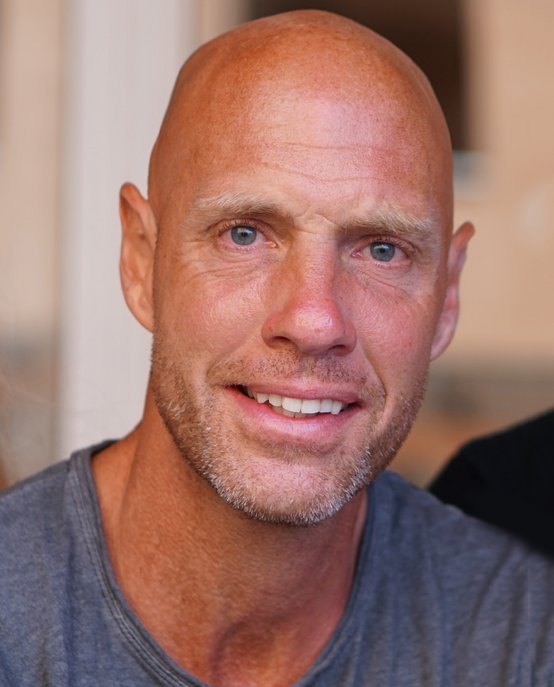 Mulder
Mulder
Professor of Precision Medicine at the department of Biomedical Engineering of Eindhoven University and Professor Radiology and Oncological Sciences at Mount Sinai’s Translational and Molecular Imaging Institute (TMII, Icahn School of Medicine, New York, USA).
Therapeutic targeting of innate immunity with nanobiologics
Immunotherapy is revolutionizing the treatment of diseases. Most of the immunotherapy strategies currently being developed engage the adaptive immune system. In recent years, emerging evidence has shown that the innate immune system displays long-term changes in its functional program through metabolic and epigenetic programming of myeloid cells (monocytes, macrophages, dendritic cells). Therefore, targeting myeloid cells and their progenitors is a powerful ‘therapeutic framework’ to regulate the delicate balance of immune homeostasis, priming/training and tolerance. This Presentation will showcase how nanobiologic-based immunotherapies can be applied to achieve long-term therapeutic benefits in detrimental diseases, including cancer and cardiovascular diseases as well as to prevent organ rejection after transplantation. In addition, a translational workflow involving innovative multimodality imaging approaches and large animal models will be discussed.
Prof. Dr. Xavier Saelens
Professor at the department of Biochemistry and Microbiology at Ghent University and Principal Investigator VIB-UGent Medical Biotechnology Center.
A universal influenza A vaccine based on the extracellular domain of the M2 protein
Influenza and human respiratory syncytial virus (RSV) infections can cause serious disease. Currently used influenza vaccines have moderate and variable efficacy, whereas there is no licensed vaccine yet against RSV. Our laboratory has focused on the highly conserved extracellular domain of Matrix protein 2 (M2e) of influenza A viruses to develop a universal influenza A vaccine candidate. Protection induced by M2e-vaccines against influenza A virus challenge is very broad and primarily mediated by non-neutralizing M2e-specific IgG that can activate Fcγ Receptors on alveolar macrophages. In vitro, this mode of protection can be mimicked and quantified in an antibody-dependent cellular phagocytosis assay using murine or human sera that contain M2e-specific IgG. More recently, we also generated M2e-targeting antibody-based biologicals with therapeutic anti-influenza A potential.The Influenza neuraminidase (NA) is a variable antigen that is largely neglected in currently used influenza vaccines. In collaboration with a private partner, we demonstrated that pan-N1 subtype NA immunity can be induced by computationally guided consensus recombinant NA antigens. In addition, we recently demonstrated that NA-specific antibodies that lack NA inhibiting activity can protect against influenza through Fc-mediated effector mechanisms.
Our lab has also explored an unconventional approach to develop a vaccine candidate against RSV by focusing on the extracellular domain of the small hydrophobic protein (SHe) of this virus. We showed that a SHe-fusion construct can induce SHe-specific antibodies that strongly reduce RSV replication in challenged mice and cotton rats. A phase 1 clinical study in older adults revealed that an adjuvanted SHe peptide vaccine was well tolerated and could induce SHe-specific IgG titers that were sustained for more than a year.
Mini lectures:
 José Borghans
José Borghans
Associate Professor of Immunology at University Medical Centre Utrecht
The quantification of T-cell dynamics
This lecture will focus on different studies on the quantification of T-cell dynamics in healthy people and laboratory animals. It shows how the quantification of T-cell dynamics has revealed a fundamental difference in the maintenance of naive T cells between mice and humans. It also addresses the dynamics of T cells in patients after stem-cell transplantation, and shows that it is questionable whether the human immune system is capable of inducing a successful homeostatic response to low lymphocyte numbers. Finally, it focusses on recent insights into memory T-cell dynamics. We show that cellular longevity is not a key characteristic of memory T cells. Importantly, insights into immunological memory in humans are almost exclusively based on studies of cells from the blood. It has recently been suggested that the bone memory provides a niche for long-lived memory T cells that hardly recirculate through the blood and therefore go unnoticed in most immunological studies.

Dr. Mieke Boots
Professor of Immunology at the Department of Rheumatology and Clinical Immunology at University Medical Centre Groningen
Ageing, Inflammaging and Immunosenescence
Age is an important risk factor for all sorts of diseases. This is because ageing has profound effects on cells and tissues of all living organisms, including those of the immune system. This lecture will introduce the concept of inflammaging, a contraction of the words inflammation and ageing, which refers to a chronic low grade inflammatory state that increases with natural ageing. In this lecture, the concept of inflammaging and its link with immunosenescence will be discussed.
Dr. Vera Kemp
Postdoc at the department of Pathobiology,
Faculty of Veterinary Medicine at Utrecht University
Exploring reovirus for use in oncolytic virotherapy
One of the anti-cancer approaches that has recently gained more attention uses oncolytic viruses. These are viruses that kill transformed cells while sparing normal cells. An example is reovirus, a non-enveloped virus harboring a genome consisting of 10 dsRNA segments. Oncolytic virotherapy using reovirus has entered a variety of human clinical trials, which demonstrated both the safety and feasibility of the approach. Several aspects of this research will be discussed, including the identification of intracellular factors that facilitate the reovirus replication cycle, genetic arming of the virus with potentially therapeutic factors, and directed evolution approaches (using selection pressure) to obtain reovirus variants with e.g. a broadened tumor tropism.
Workshops:
Erik Ensing
Senior Director Business Development at Lava Therapeutics
Erik Ensing obtained his MSc in Biology at the University of Utrecht in 2001. He decided not to pursue a PhD position, but to make a career in the biotech industry. Early 2002 he started as a Research Associate (technician) in the lab of Genmab, a Danish biotech company developing therapeutic antibodies. Over a period of almost 16 years he worked in 6 different positions. At the end of his Genmab career he was Director Alliance Management and, amongst others, responsible for managing the daratumumab Alliance between Genmab and Janssen. January 2018 he became the second employee and senior business developer of Lava Therapeutics (LAVA), a start up company that is developing bispecific antibody T cell engagers for the treatment of cancer. LAVA now has 17 employees, is running its own lab to support preclinical development and is progressing two compounds towards the clinic.
Prof. Dr. Leo James
MRC Programme Leader, Medical Research Council Laboratory of Molecular Biology.
Leo received his Ph.D. from Cambridge University in 2000 and post-doc’d with Prof. Dan Tawfik and Sir Greg Winter, on antibody structure, function and evolution. In 2007, Leo established a lab at the LMB in Cambridge studying host-pathogen interactions using a broad range of in vitro and in vivo techniques. In 2010, Leo discovered TRIM21, the most conserved and highest affinity antibody receptor in mammals and uniquely cytosolically expressed. Since then, his lab has shown that TRIM21 prevents infection by intercepting viruses, bacteria and pathogenic proteins inside the cell and targeting them for rapid degradation. This work has also led to the development of ‘TrimAway’, a technique which exploits TRIM21 for the rapid and specific degradation of cellular proteins. Leo also investigates HIV post-fusion biology; recent work includes identifying the HIV capsid interface used to recruit import cofactors and dynamic pores in the capsid that are essential for HIV infection.
Kristin Strumane
Assistant Director and Scientific Writer at Genmab
Kristin Strumane is Assistant Director, Translational Research at Genmab, where she is responsible for the nonclinical pharmacodynamics documentation that is required for regulatory filings to start clinical trials. Kristin has a background in molecular biology and obtained her PhD at the University of Ghent, Belgium. She worked for four years as a postdoctoral researcher at the Netherlands Cancer Institute (NKI) in Amsterdam. Thereafter, she was recruited to work for some time with Prof. C. Melief for ISA Pharmaceuticals at the LUMC in Leiden, where she gained experience in the field of immunology. In 2008 she started as Scientific Writer at Genmab in Utrecht, where she is still happy and intrigued by this very special molecules called antibodies.
